Pap Smear
Once you turn 21 or become sexually active, you should get regular Pap smear tests. The Pap Smear test is a routine part of a yearly gynecological exam, along with a breast exam, palpation of your abdomen, and a discussion with your gynecologist. Abnormal pap smears should always be evaluated with a thorough consultation and examination by a physician for an accurate diagnosis and treatment plan. It may be a sign of a serious illness or condition.
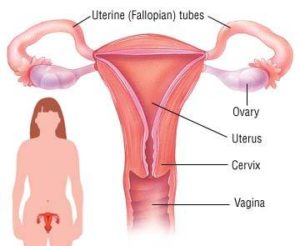
While performing a Pap smear, your gynecologist actually brushes cells from your cervix after inserting a speculum in your vagina. The tissue samples then are sent to a lab to be analyzed. Pap smears allow your doctor to track any changes in your cervix, which could be indicative of several things, including cancer.
The Pap smear results may contain any of the following:
- Normal cells
- Abnormal cells
- Presence of the human papillomavirus (HPV)
Normal cells constitute a negative result. Abnormal cells, and even the presence of HPV, can tell your local gynecologist several different things. A Pap smear allows your doctor to catch conditions in a very early stage — before the development of cervical cancer. Luckily, this is a very slow-growing form of cancer, so it can take years before it becomes life-threatening.
Pap smear recommendations frequently change. So make sure to always ask your gynecologist for the most current recommendation on screening.
Gynecologist of Manhattan Women’s Health & Wellness offers comprehensive Obstetrics & Gynecology care in New York City for women of all ages. At our OBGYN clinic, we provide a full range of gynecology services, from annual check-ups and routine pap smears to the treatment of Menstrual Cramps and GYN procedures, surgeries performed in our office or the hospital. Visit our state-of-the-art women’s center to experience the best gynecology NYC has to offer.
Abnormal Cells Are Not All the Same
Your Manhattan OBGYN may find many potentially dangerous results from a Pap smear test:
- Atypical squamous cells of undetermined significance (ASCUS). These squamous cells normally are present on your cervix as thin, flat cells. Sometimes, though, a Pap smear reveals that some of the squamous cells are abnormal. At this point, your doctor can re-analyze the same sample, looking for viruses that are indicators of cancer.
- Squamous intraepithelial lesion. This result points to changes that could indicate a very early form of a potentially precancerous condition. Depending on what else may be present in your Pap smear test results, such as HPV, these lesions can have a greater or lower impact. There are two types:
- Low grade. These are minor changes in characteristics such as the size and shape of the lesion, indicating that pre-cancerous cells, if present, are many years away from potentially developing into cancer.
- High grade. These are changes that indicate a precancerous abnormality may be present, and further testing is necessary.
- Atypical glandular cells. Glandular cells produce mucus, and they’re found in both the uterus and the cervix. These cells can sometimes look irregular. Although gynecologists aren’t sure what this indicates, there’s no clear correlation between these abnormal cells and cancer. Typically, your gynecology doctor orders more testing to develop a diagnosis.
- Squamous cell cancer (or adenocarcinoma cells). This result refers to two different types of cancer that are almost certainly present:
- Squamous cells reside in the cervix. Therefore, Squamous cell cancer indicates the presence of cancer in the cervix.
- Adenocarcinoma cells indicate that the glandular cells in either the uterus or the cervix are cancerous.
Seeking a Diagnosis

In order to find a diagnosis, your gynecologist does one of the following, depending on your Pap test results:
- Repeat the Pap smear test. The possibility exists that there could be a simple reason for the abnormal cells. For example, blood or other physical factors could have been in the way, which kept your OBGYN gynecologist from getting a clean swipe of cells. Your gynecologist may want to repeat the test immediately or — depending on your age, previous Pap test results, and medical history — ask you to come back in three months, six months, or even a year.
- HPV testing. Another possibility is that HPV cells were present, causing the abnormal result. In this case, your doctor may want you to take one of two HPV tests:
- Reflex HPV testing. In this test, your doctor uses the same cell sample from the initial swab taken during your routine Pap smear. The lab looks for any type of HPV. Of the more than 16 different varieties, only a few normally lead to cervical cancer. Those are the types gynecologists and the lab will be looking for.
- HPV typing test. This test looks for the specific type of HPV, for example, looks for HPV 16 and HPV 18, the most common types of HPV that lead to cervical cancer. It’s a more limited test, but it’s accurate in discovering the most likely types of HPV.
Once the type of HPV on your cervix is determined, treatment for your symptoms can be arranged. There is no HPV treatment, but if you’re diagnosed with it, you may experience a range of symptoms, all of which are treatable. Again, your gynecologist selects the most appropriate treatment based on the type of HPV you have and what your symptoms are. Symptoms can include genital warts, cervical pre-cancer, and other cancers caused by HPV.
- Colposcopy: This procedure allows your OBGYN in NYC to closely examine the tissues of your cervix, vulva, and vagina with a special magnifying microscope. While using the colposcope, your doctor may also opt to take a biopsy — that is, a small piece of the abnormal tissue. This procedure could mean some post-procedure discomfort for you, such as cramping and light bleeding.
- Endocervical curettage: In this case, the doctor has to insert a small tool to take a scraping of the cells inside the cervix. This procedure may result in some cramping or bleeding.
- Cone biopsy: This type of biopsy can also be a treatment if the area of abnormal cells is small. In this instance, a cone-shaped section of the cervix is removed, potentially taking all the abnormal cells with it. This allows the healthy cells to grow back.
Getting ready for a Pap and/or HPV Test in Midtown, Manhattan
There are several steps you can take to ensure that you get the best results possible from an HPV or Pap test:
- Avoiding sexual intercourse two days (48hrs) before the test
- Schedule the test on a day when you are not on your menstrual cycle
- Avoid taking a shower 48 hours before the test
- Avoid the use of tampons, vaginal creams, films, foams, or any vaginal pessaries inserted into the vaginal canal for at least 48 hours before the test.
An Important Step in Your Life
Pap smear tests are the first line of defense against cancer and many other treatable conditions for all women. It’s a safe and simple procedure you should have done regularly — and during prenatal care to ensure the health and safety of you and your baby.
Have questions about Abnormal Pap Smear? Would you like to schedule an appointment with a top OB\GYN doctor and a leading pap smear specialist on the Upper East Side or Midtown, Manhattan? Please call our office today.
Updated on Sep 23, 2023 by Manhattan Women’s Health and Wellness
Best-in-class
New York Gynecology Clinic
Manhattan Specialty Care in the Press

Call now to make an appointment with our highly rated Manhattan Gynecology doctors regarding your health. We look forward to seeing you!
book online now
(212) 378-9985
New York City Locations:
Manhattan Women's Health & Wellness (Upper East Side)
983 Park Ave, Ste 1D17
New York, NY 10028
(212) 389-1904
Manhattan Women's Health & Wellness (Midtown)
56 W 45th St, Ste 815
New York, NY 10010
(212) 677-7654
Manhattan Women's Health & Wellness (Union Square)
55 W 17th St, Ste 104
New York, NY 10011
(212) 378-9985