Pelvic Pain
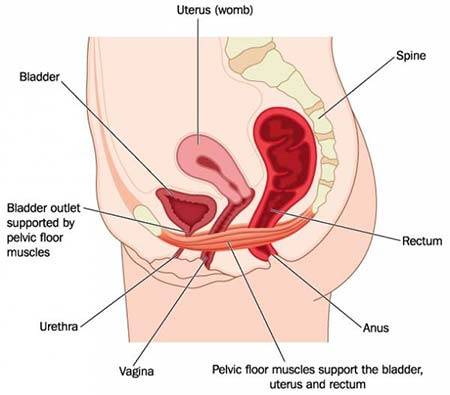 Pelvic pain refers to the discomfort and pain you may feel in the lower abdominal area of your body. The pain may not stay there and can radiate into your lower back, buttocks, and thighs, depending on the cause or source of the pain. Pelvic pain in women is most often stems from the reproductive system, digestive system, urinary system, or musculoskeletal system. Pelvic pain should always be evaluated with a thorough consultation and examination by a physician for an accurate diagnosis and treatment plan. It may be a symptom or sign of a severe illness or condition.
Pelvic pain refers to the discomfort and pain you may feel in the lower abdominal area of your body. The pain may not stay there and can radiate into your lower back, buttocks, and thighs, depending on the cause or source of the pain. Pelvic pain in women is most often stems from the reproductive system, digestive system, urinary system, or musculoskeletal system. Pelvic pain should always be evaluated with a thorough consultation and examination by a physician for an accurate diagnosis and treatment plan. It may be a symptom or sign of a severe illness or condition.
Pelvic pain symptoms vary greatly because there are numerous possible causes. Pain can be caused by:
- Dull or sharp
- Intermittent or constant
- Mild, moderate, or severe
- Localized — that is, in one specific area, as opposed to radiating pain
- Sudden, built over time, acute, sharp, or constant — constant pain is associated with chronic pain, which is pain that has been present for a longer time
- Present only with specific movements or situations, such as pelvic pain during sex
- Described as pelvic cramps
If the pain is acute and persistent, you should make an appointment to see the gynecologist, or your local ob-gyn doctor right away.
Gynecologist of Manhattan Women’s Health & Wellness offers comprehensive Obstetrics & Gynecology care in New York City for women of all ages. At our ob-gyn clinic, we provide a full range of gynecology services, from annual check-ups and routine pap smears to Pelvic Pain treatment and GYN procedures. Our state-of-the-art gynecology facility has the latest technologies.
What Causes Pelvic Pain?
Since pelvic pain can stem from one of several systems, there are a variety of causes, usually narrowed down by pain type, including:
- Appendicitis
- Fibromyalgia
- Inguinal hernia
- Kidney stones
- Prostatitis
- Urinary tract
- Colon cancer
- Chronic constipation
- Crohn’s disease
- Diverticulitis
- Painful bladder syndrome
- Irritable bowel syndrome
- Pelvic floor muscle spasms
- Ulcerative colitis
- Past physical trauma, abuse, or sports injuries
- Past sexual abuse
Female Pelvic Pain
A woman may experience pelvic pain deriving from the reproductive system. It can stem from:
- Adenomyosis, which is when cells from the uterine wall begin growing within the uterine muscle itself, continuing to grow, break down, and shed every month, causing pain and periods that are heavy and painful
- Endometriosis, when cells from the uterine wall, called the endometrium, grow outside the uterine wall. This condition often is excruciating. It can also impact other organs, such as your ovaries, fallopian tubes, and the tissues of your pelvic area.
- Menstrual cramps, which can present as sharp pain in the vaginal area
- Ectopic pregnancy is a common cause of pelvic pain during pregnancy and happens when a fetus begins developing in your fallopian tubes
- Ovulation pains, which differ from appendicitis pains; this pain characterizes as lower left abdominal pain in women, as opposed to the pains on the right felt with appendicitis
- Ovarian cysts or cancer
- Pelvic inflammatory disease (PID), a sexually transmitted bacterium that spreads from your vagina into the female reproductive organs; PID is often present without symptoms.
- Uterine fibroids
- Vulvodynia, or chronic vaginal pain without a clear root cause
- Vaginitis, an inflammation of your vagina that a viral infection can cause, an STD, or a yeast infection
- Vaginismus, whereby anything that enters the vagina causes pain, even when trying to use a tampon or during a medical exam
Testing for Pelvic Pain

Your gynecologist will begin by performing a physical exam during your visit to see if he can determine the cause of the pain with any tests. At the very least, he should rule out the systems that aren’t the source. There are routine tests, like blood tests, urinalysis, a pregnancy test, and a Pap smear. If those don’t reveal a diagnosis, your doctor moves onto:
- Ultrasound, which allows your GYN to see your internal organs via sound waves
- CT scan uses X-rays in combination with computer technology to see your organs in a cross-section as slices.
- MRI, which produces two-dimensional images of your organs
- Laparoscopy, classified as a minor surgical procedure, where small incisions are made in your abdominal wall so that the specialist can insert a lens and light to see any endometrial growths
- X-rays or a picture of your bones and organs
- Colonoscopy, a routine procedure that every person will require at some point. It uses a small camera to look at the inside of your intestines
Diagnosis and Treatment
Once your gynecologist has run tests and checked each of your systems carefully, they should be able to either give you a precise diagnosis or refer you to a specialist. When the cause is within your reproductive system, your gynecologist may prescribe pain medications, antibiotics, or surgery where necessary.
The specialist may ask you to try oral contraceptives if the pain is hormone-related or related to your menstrual cycle. A physician should evaluate pelvic pain with a thorough consultation and examination for an accurate diagnosis and treatment plan. It may be a symptom or sign of a severe illness or condition, and your doctor should perform a careful follow-up.
Women often experience pelvic pain, and sometimes there isn’t a cause that a doctor can discern. In those cases, the specialist may recommend you to try anti-inflammatory or pain relief medication, relaxation exercises, or physical therapy.
There are many new treatments for pelvic pain that have promising results.
Your treatment also may involve a multi-pronged approach of dietary changes, exercise, stress relief, or even environmental changes. If none of these treatments seems to help, you may come away with the diagnosis of chronic pelvic pain syndrome (CPPS). CPPS classifies as pelvic pain that has been present for several months and does not respond to treatment.
Have questions about Pelvic Pain? Schedule an appointment with the best-rated OBGYN in Manhattan and the top pelvic pain treatment specialist in New York City (Midtown and Upper East Side).
Updated on Sep 23, 2023 by Manhattan Women’s Health and Wellness
Best-in-class
New York Gynecology Clinic
Manhattan Specialty Care in the Press

Call now to make an appointment with our highly rated Manhattan Gynecology doctors regarding your health. We look forward to seeing you!
book online now
(212) 378-9985
New York City Locations:
Manhattan Women's Health & Wellness (Upper East Side)
983 Park Ave, Ste 1D17
New York, NY 10028
(212) 389-1904
Manhattan Women's Health & Wellness (Midtown)
56 W 45th St, Ste 815
New York, NY 10010
(212) 677-7654
Manhattan Women's Health & Wellness (Union Square)
55 W 17th St, Ste 104
New York, NY 10011
(212) 378-9985