Hysteroscopy
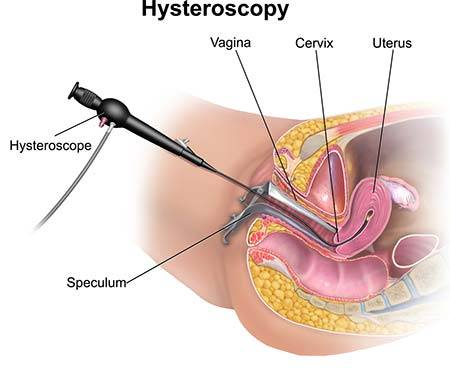 Hysteroscopy refers to any diagnostic or therapeutic procedure in which your doctor employs a hysteroscope. A hysteroscope is a thin tube with an expandable light at the end.
Hysteroscopy refers to any diagnostic or therapeutic procedure in which your doctor employs a hysteroscope. A hysteroscope is a thin tube with an expandable light at the end.
Gynecologists can use the device as a diagnostic tool — that is, to assist in an examination on the way to making a diagnosis — or as a functional tool to aid in a surgical procedure.
Similar to a laparoscope, a hysteroscope allows your doctor to examine inside your vagina and uterus. Laparoscopy is a procedure that allows your doctor to examine the outside of your uterus with a laparoscope. When your doctor examines the inside of your uterus with a hysteroscope, this is referred to as hysteroscopy.
Our doctors employ both devices, laparoscope, and hysteroscope simultaneously to obtain a complete picture of your uterus, both inside and out.
Hysteroscopies can be both diagnostic and therapeutic
Why Do You Need a Diagnostic Hysteroscopy?
Even with a speculum in place, it may have difficulty seeing past your cervix into your uterus. A lighted hysteroscope makes the process easier. The camera allows image lighting and magnification.
Reasons for a diagnostic hysteroscopy include:
- Abnormal bleeding, especially after menopause
- An abnormal Pap smear result
- Uterine bleeding
- Trying to diagnose infertility causes
- Diagnosing pain symptoms
Your physician can use it to assist in other ob-gyn procedures, as well. For example, your doctor may simultaneously use a diagnostic hysteroscopy and laparoscopy. Or they can use it to ascertain the position of your uterus before a uterine suspension. Because it’s so versatile, the hysteroscope has become a commonly used tool in a doctor’s toolbox.
Why Do You Need a Functional Hysteroscopy?

Because the hysteroscope is a hollow tube, your gynecologist in Midtown, Manhattan, and Upper East Side can pass tools through it to perform functional tasks. The two uses of a hysteroscope go hand-in-hand, as its diagnostic use can find an issue — such as endometrial polyps — and its practical use can perform the task, in this case removing the polyps (a hysteroscopy polypectomy).
Your gynecologist accomplishes this by pushing a cutting tool through the hysteroscope to remove the polyps.
Other functional hysteroscopy uses include:
- Identifying and removing uterine fibroids
- Removing genital warts
- Finding and removing adhesions
- Taking a hysteroscopy biopsy
- Removing an IUD (an intrauterine device used for contraception)
- Locating the cause of abnormal bleeding and sealing it (hysteroscopy ablation)
What Are the Pros and Cons of Hysteroscopy?
Every tool your gynecologist uses and every procedure pose some risk. Often, the healing benefits outweigh the medical risks, but your gynecologist should explain everything to you well enough to weigh the pros and cons yourself.
With hysteroscopy, there are substantial benefits, including:
- It’s a minimally invasive procedure.
- It leads to a much shorter recovery period.
- You’ll need less pain management (and fewer drugs).
- You’ll rarely if ever, need a hospital stay after hysteroscopy.
- You can avoid more intensive and invasive surgery.
The risks and side effects associated with hysteroscopy are similar to other gynecological procedures:
- Introducing an infection
- Causing heavy bleeding
- Accidentally damaging your bladder, bowels, cervix, or uterus
- Scarring of the endometrium (the lining of your uterus)
- Creating unexpected problems from the gas or liquid used to expand your uterus
Furthermore, you should not have a hysteroscopy done if you’re pregnant or suffering from:
What Happens During the Hysteroscopy Procedure?
A hysteroscopy is almost always an outpatient procedure. The doctor performs most of them in a specialized Women’s Health Care center. When your OBGYN performs a hysteroscopy, both diagnostic and functional uses are both employed. Depending on the purpose and goal of the procedure you’re undergoing, you may need general anesthesia or just mild sedation with local anesthesia. Make sure you know which you will receive before you agree to the procedure so that you can make appropriate plans for your recovery once you get home.
Here’s a common procedure as a sample:
- Your Midtown gynecologist dilates your cervix, inserts the hysteroscope into the vagina, passes the cervix, and reaches your uterus after you’re situated.
- A gas, like carbon dioxide, or a liquid, like saline, is passed through the hysteroscope into your uterus to clean it out and expand it.
- The lighted end of the tool lets your doctor examine in detail inside your uterus, including where the fallopian tubes branch off.
- If you need to undergo the procedure — whether a biopsy, ablation, or polypectomy — your physician can pass the appropriate tool through the hysteroscope to exactly where it is is needed.
Your procedure can take anywhere from five minutes to an hour, depending on what you’re having done. Ask gynecologist before the procedure to explain anything you don’t know or understand, including how long your process should take.
What Should I Know About Hysteroscopy Recovery?
You rarely need to do anything special after a hysteroscopy since it’s so minimally invasive. However, depending on the specifics of your procedure, you may experience some cramping or light bleeding for several days. You can take a mild pain reliever (except aspirin, which can increase bleeding) as needed.
Your gynecologist may advise you not to douche or have sexual intercourse for two weeks after your hysteroscopy. Still, you can return immediately to all your other normal daily activities without limitations. You can even eat your regular diet right after your procedure. Just remember that you may be a little gassy.
Hysteroscopies require minimal recovery, usually just one day
Which Hysteroscopy Notes Exist?
Regardless of the purpose of your hysteroscopy — even if it was a functional procedure — you should have no problems trying for pregnancy after hysteroscopy. Some fertility clinics use hysteroscopy procedures to determine the cause of infertility and correct it, if possible.
If you have severe pain, a fever, heavy bleeding, an unusual discharge, or spotting after hysteroscopy, contact your gynecologist in Midtown. These are abnormal reactions to the procedure and may indicate a rare complication.
Your gynecologist should evaluate symptoms with a thorough consultation and examination for an accurate diagnosis and treatment plan to exclude any serious underlying condition.
How Safe Is a Hysteroscopy?
All surgeries are not entirely safe, and in different cases, there can be complications. Statistics say that less than one percent of all patients risk experiencing infection, heavy bleeding, intrauterine scarring, etc. Your doctor can perform this operation only if the benefits outweigh all the risks.
Can I Eat or Drink Before a Hysteroscopy?
You can eat something light, like a soup or salad, but this meal should be the night before the procedure. It is prohibited to eat or drink on the day of the treatment.
Have questions about Hysteroscopy? Schedule an appointment with the best-rated NYC Gynecologist today.
Updated on Sep 23, 2023 by Manhattan Women’s Health and Wellness
Best-in-class
New York Gynecology Clinic
Manhattan Specialty Care in the Press

Call now to make an appointment with our highly rated Manhattan Gynecology doctors regarding your health. We look forward to seeing you!
book online now
(212) 378-9985
New York City Locations:
Manhattan Women's Health & Wellness (Upper East Side)
983 Park Ave, Ste 1D17
New York, NY 10028
(212) 389-1904
Manhattan Women's Health & Wellness (Midtown)
56 W 45th St, Ste 815
New York, NY 10010
(212) 677-7654
Manhattan Women's Health & Wellness (Union Square)
55 W 17th St, Ste 104
New York, NY 10011
(212) 378-9985