If you’re weighing the copper IUD vs. Mirena, consult your local ob-gyn specialist in NYC or gynecologist. While the copper version lasts longer, the Skyla is smaller. All have their advantages and issues. All of them are equally effective birth control devices. You should discuss all options and your specific case with your NYC gynecology provider.
Intrauterine Device (IUD)
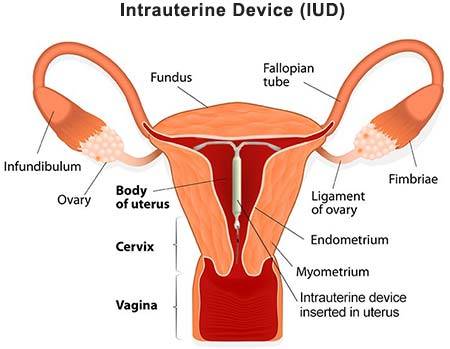 The intrauterine device, most commonly referred to as an IUD, is a form of birth control. Shaped like a small “T,” it’s placed in your uterus by your doctor or healthcare provider. Your cervix then holds it tightly in place. IUD effectiveness is unchallenged; the intrauterine device failure rate is less than 1 percent. In fact, according to the U.S. Department of Health and Human Services, this method is more effective at birth control than the pill, the vaginal ring, the patch, and prophylactics.
The intrauterine device, most commonly referred to as an IUD, is a form of birth control. Shaped like a small “T,” it’s placed in your uterus by your doctor or healthcare provider. Your cervix then holds it tightly in place. IUD effectiveness is unchallenged; the intrauterine device failure rate is less than 1 percent. In fact, according to the U.S. Department of Health and Human Services, this method is more effective at birth control than the pill, the vaginal ring, the patch, and prophylactics.
Despite their effectiveness and safety, fewer than five percent of women under 30 use them. Part of the reason is misinformation about the IUD insertion process. We will address all the concerns below, but consider getting an intrauterine device if you want an effective birth control method.
Overall evidence suggests that the risk of adverse outcomes related to pregnancy, perforation, infection, heavy bleeding, or removals for bleeding among young IUD users is low and may not be clinically meaningful. IUDs are safe for young women and provide highly effective reversible contraception.
ParaGard vs Mirena
Two types of IUDs exist, and there are three leading brands available. Talk to your GYN specialist about which might be best for you:
- Nonhormonal IUDs (ParaGard) are wrapped with copper
- Hormonal IUDs (Mirena and Skyla) use the hormone progestin
The non-hormonal intrauterine devices emit copper ions that kill or confuse sperm cells. They are hormone-free and can last 10 to 12 years. Since they are chemical-free, they don’t disrupt your normal menstrual cycle like other forms of birth control. You can even insert one up to five days after unprotected sex as an emergency contraceptive.
The hormonal IUDs can last from three to five years, depending on the brand you use. Skyla is smaller than Mirena, but otherwise, they’re the same. Every day, the device releases a small amount of progestin, creating a plug of mucus at your cervix that prevents sperm from passing.
Facts About IUD Insertion
You can get an intrauterine device only from a gynecologist and an ob-gyn specialist because a doctor can insert it correctly. Inserting it takes less than a minute in the gynecology office. The intrauterine device insertion process is comparable to getting a pap smear with some accompanying cramping. Some women experience lightheadedness or nausea, but it’s rare. The procedure can be temporarily uncomfortable, but most women who use this option say the discomfort is worth it for years of easy birth control.
The best way to prepare is to educate yourself. Your gynecologist uses a speculum to see into your vagina. After cleaning your vagina and cervix, your healthcare provider may measure how deep your uterus is to ensure that the IUD fits. Then the device is inserted into your uterus using an applicator tube. After your doctor removes it and cuts the strings of the intrauterine device, you’re finished.
IUD Side Effects
While your gynecologist has to insert the device, it’s virtually maintenance-free. IUD complications are rare, and the side effects are minimal. Most subside after several months. Issues can include:
- With a ParaGard IUD, your periods might get a little worse for a few months before subsiding.
- With a Mirena or Skyla IUD, you may notice spotting for up to six months, but then your period should lighten, meaning it becomes a light flow for a couple of days.
- You may experience breast tenderness, mood shifts, or increased acne for a few months, but all these symptoms fade over time.
- You may get an IUD infection in your pelvic area within three weeks of inserting the device, but it’s not at all common.
- Regardless of which intrauterine device you choose, there is a three percent chance that it will dislodge and come out of your uterus. The dislodging of the device won’t affect your health, but it leaves you unprotected until you have it re-inserted.
The Ideal Candidate for the Intrauterine Device (IUD)
The vast majority of women can make use of an IUD. IUDs are more applicable to women with one partner and low risk of being exposed to STDs. However, it is essential to remember that an intrauterine device does not protect you from sexually transmitted diseases. You cannot utilize an intrauterine device if:
- You are suffering from STD or had a recent pelvic infection
- You have cancer of the uterus or cervix
- You are pregnant
- You have unexplained vaginal bleeding
Furthermore, you should use an IUD if you have an allergy to copper or suffer from Wilson’s disease that makes your body hold too much copper. Liver disease and breast cancer are additional contraindications for hormonal IUDs. Your doctor will also consider your uterus’s shape and size when determining whether you are a good candidate for an intrauterine device. In rare cases, the factors mentioned above can make it difficult to place an IUD.
IUD Pros and Cons
Like all contraception methods, IUDs provide benefits but there are some risks. Consider:
Pros
- It represents a completely reversible form of birth control.
- They start working as soon as they’re inserted.
- Compare IUD vs. pill, and IUD is often the better choice. You have to remember to take medicine every day while the IUD is maintenance-free. Additionally, intrauterine devices are more effective.
- IUDs also reduce the likelihood that an embryo can attach to your uterine wall, further lessening the chance of pregnancy.
- You can use the copper IUD as an emergency method to prevent pregnancy if inserted within five days of your unprotected sex.
- Hormonal IUDs ease menstrual cramps and make your periods lighter.
- With copper IUDs, your period might disappear altogether.
Cons
- You must visit a gynecologist or a family planning clinic to get an IUD. Only a gynecologist can insert one.
- IUDs do nothing to prevent sexually transmitted diseases and infections.
- The insertion procedure can be uncomfortable for some women.
- You have to be comfortable with the idea of inserting a device into your uterus.
- The hormonal intrauterine devices release chemicals into your bloodstream. As a result, you may experience unusual cramping or IUD bleeding, at least temporarily.
- The device can fall out of your uterus, although it’s rare that this happens. But if the device isn’t in your uterus, it can’t protect you and needs to be re-inserted by a gynecologist.
- The instance of IUDs coming loose from your uterus is increased for women:
- Younger than 20 years old
- Who have never been pregnant
- Have a history of severe cramping and a heavy flow
- Who has had their IUD fall out in the past
Placing an IUD
Your doctor will typically place an intrauterine device during an office appointment. Generally, your healthcare provider will prescribe you over-the-counter medications such as ibuprofen. You should take them a few hours before the procedure to offset cramping.
The beginning of the procedure is similar to undergoing a PAP smear. Your doctor will place your feet in stirrups and will put a speculum in the vagina. The specialist will typically do it to keep the vagina open. The next step is placing an IUD in a small tube and inserting it into your vagina. Your doctor will then move it up through the cervix and into the uterus. In the end, they will push an IUD out of the tube and pull both out. Keep in mind that the strings attached to the IUD will hang 1-2 inches into the vagina.
Patients report that the procedure can be pretty uncomfortable, and you might experience bleeding and cramps. However, these issues tend to disappear within a few days after your doctor completes the process. The specialist can place an IUD at any time in your cycle. Although, you should have an intrauterine device placed while you are on your period since it is when your cervix is most open.
Sex After IUD Insertion
While the birth control efficiency of the intrauterine device is unmatched, the ultimate question is whether the device negatively affects sex. Your partner may feel the strings left on the device, these strings soften with time, and the feeling is not painful at all.
Some women report that their sex has improved because IUD removes any worry about an unwanted pregnancy. Of course, your experience may differ, but using a worry-free contraceptive — and one that you can reverse entirely at any time — offers women the freedom they seek.
Final Words
According to the National Institutes of Health, no scientific evidence suggests that using an intrauterine device — whether the ParaGard, Mirena, or Skyla — leads to IUD weight gain. Numerous studies point to no unwanted weight gain at all.
Consult your local ob-gyn specialist if you’re weighing the copper intrauterine device. While the copper version lasts longer, the Skyla is smaller. All have their advantages and issues. All of them are equally effective birth control devices. You should discuss all options and your specific case with your gynecologist.
Frequently Asked Questions
What is an intrauterine device?
An intrauterine device, commonly referred to as IUD, is a small T-shaped device placed in the uterus by your healthcare provider. The main goal of this tiny device is to prevent pregnancy. According to several reputable studies, IUD is considered one of the most effective birth control methods on the market. There are currently two types of IUDs: the hormonal-levonorgestrel IUD and the non-hormonal-copper T IUD.
How does an intrauterine device (IUD) work?
Both hormonal and non-hormonal IUDs aim to prevent pregnancy by modifying how sperm cells move to avoid getting to an egg. One of the most significant advantages of IUDs is that they can last for years, and whenever you decide to get pregnant, your gynecologist can quickly and easily remove them.
Can an intrauterine device prevent transmitted diseases?
A lot of people have a misconception that IUDs can protect them from transmitted diseases. Unfortunately, that is not true. The experts have already proved that intrauterine devices do not protect a woman from sexually transmitted diseases (STDs). Couples who are having sex must always use condoms in conjunction with IUD to protect themselves from STDs. Keep in mind that before putting in an IUD, you should get checked for sexually transmitted diseases.
Do you need a prescription for an intrauterine device?
Yes, you need to obtain a prescription to get an IUD. A qualified specialist should insert this small device. Before prescribing an IUD, your healthcare provider will make you aware of all the potential side effects that may occur, such as irregular periods, severe menstrual cramps, etc. Although, these side effects typically disappear once your body adjusts to the IUD.
How long does an IUD last?
Everything depends on the type of device you get. For instance:
- Skyla – 3 years
- Mirena, Liletta, and Kyleena – 5 years
- ParaGard – 10 years
Will I experience a change in my periods?
According to several reputable studies, many women with hormonal IUDs experience fewer cramps. Additionally, during the first few months, a woman might have irregular spotting. When it comes to ParaGard, they can make your cramping worse and your periods heavier. However, these complications might disappear after a few months.
Will my partner feel like an intrauterine device?
Generally, your partner should not be able to feel your intrauterine device. Even if he does, it will be a minor contact with the strings of the IUD, which is not supposed to cause any discomfort. The longer you have an IUD, the softer they become. Moreover, the doctor can trim the strings upon a patient’s request.
Is it possible for an intrauterine device to fall out?
During your regular gynecologist visits, your doctor will check your device. Your cervix is supposed to hold the intrauterine device in place. However, in rare cases, it can fall part of the way or part of the way. You are running a higher risk of an IUD falling out if:
- You are under 20 years old
- You have fibroids in your uterus
- The size and shape of your uterus is unusual
- Your IUD was placed right after having a baby or a second-trimester abortion
Can an IUD be removed?
Yes, your doctor can easily remove an IUD at the office. The whole procedure is going to take a few minutes. To remove the intrauterine device, your gynecologist will use forceps to pull it out slowly. Once your doctor completes the process, you might experience some bleeding and cramping that should go away in 1-2 days.
How soon does an IUD start working?
If your doctor inserts the hormonal IUD during your period, it starts working right away. Otherwise, this option might take up to 7 days to be effective. Keep in mind that the non-hormonal intrauterine device becomes effective as soon as the specialist places it.
Do you have questions about IUD Birth Control or intrauterine device insertion procedure? If you would like to schedule an appointment with an internationally recognized OBGYN doctor of Manhattan Women’s Health and Wellness, please contact our office for OBGYN consultation.
Updated on Sep 23, 2023 by Manhattan Women’s Health and Wellness
Best-in-class
New York Gynecology Clinic
Manhattan Specialty Care in the Press

Call now to make an appointment with our highly rated Manhattan Gynecology doctors regarding your health. We look forward to seeing you!
book online now
(212) 378-9985
New York City Locations:
Manhattan Women's Health & Wellness (Upper East Side)
983 Park Ave, Ste 1D17
New York, NY 10028
(212) 389-1904
Manhattan Women's Health & Wellness (Midtown)
56 W 45th St, Ste 815
New York, NY 10010
(212) 677-7654
Manhattan Women's Health & Wellness (Union Square)
55 W 17th St, Ste 104
New York, NY 10011
(212) 378-9985