 Urinary incontinence is the loss of control of your bladder. It can occur for several different reasons. While it’s a fairly common condition, it can cause embarrassment, leading people to keep their symptoms to themselves.
Urinary incontinence is the loss of control of your bladder. It can occur for several different reasons. While it’s a fairly common condition, it can cause embarrassment, leading people to keep their symptoms to themselves.
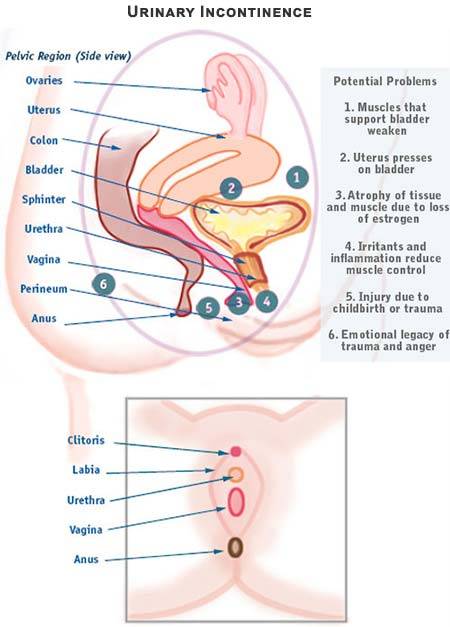
Causes of urinary incontinence can include:
- Bladder muscles are weak
- Spastic or overactive muscles
- Damaged nerves around your bladder
- Medications
The specialist should evaluate your urinary incontinence with a thorough consultation and examination by your local gynecology specialist for an accurate diagnosis and treatment plan to exclude any serious underlying condition.
Symptoms and Risk Factors of Urinary Incontinence
Urinary continence can occur with a wide range of severity. You may find that the need to urinate comes upon you suddenly, with urgency and frequency. You may find it challenging to get to the bathroom in time; accidents aren’t unusual.
While incontinence can occur due to aging, not everyone experiences it as they get older. There’s a more significant link between gender and incontinence than between age and incontinence. For example, prostate problems put men at greater risk for incontinence.
For women, urinary incontinence often develops following a pregnancy. You may experience it during pregnancy, and if so, your chances of having it continue after pregnancy increase. Some women only experience it after they’ve given birth. The risk of incontinence increases with each childbirth. Additionally, post-menopausal women are also at greater risk.
General urinary incontinence risk factors for both genders include:
- Parkinson’s disease
- Multiple sclerosis
- Alzheimer’s disease
- Arthritis
- Stroke
- Certain medications
- Nerve damage as a result of injury or surgery, especially to the spinal cord
Your doctor should evaluate all symptoms with a thorough consultation and examination by your gynecology specialist for an accurate diagnosis and treatment plan to exclude any serious underlying condition.
Types of Incontinence
There are several different types of incontinence, although it’s considered a symptom for other conditions, not a disease in and of itself. Because of this, it’s neither hereditary nor guaranteed to happen with age.
Types of incontinence can include:
- Stress Urinary Incontinence (SUI) is a result of weak pelvic muscles. Because the pelvic floor muscles are weak or stretched out, leakage occurs. Stress incontinence mainly affects older women. SUI happens during physical activity, which puts pressure on your bladder, causing the leak. This issue may occur during exercise, walking, bending or lifting, or even sneezing, coughing, or laughing. The leakage may be mild, moderate, or severe, ranging from just a few drops of urine up to a tablespoon, sometimes more.
- Overactive Bladder (OAB) happens when your brain tells your body that you need to empty your bladder when it doesn’t have enough fluid. You may feel a very abrupt urge to go that you can’t ignore, or you may end up experiencing a constant need to urinate, whether it’s day or night. With OAB, you may tend to stay home or limit your activities to be near a bathroom. You may find it hard to sleep at night with the urge to go disrupting your sleep patterns. This type of bladder incontinence shows up more in menopausal women.
- Mixed Incontinence happens when you experience both stress urinary incontinence and overactive bladder at the same time. In this condition, there are moments when strong urges to urinate frequently occur and other times when bladder leaks happen due to some activity.
- Overflow Incontinence is from a bladder that always thinks it has more fluid than it can handle and leaks pretty regularly. Additionally, you may find it difficult to empty your bladder. These issues could be due to a blockage or the bladder muscle’s inability to contract and empty the bladder fully. As a result, there are “dribbles” or leaks as your bladder attempts to release some of the pressure of what it thinks is a full bladder. This problem is rare in women and much more common in men with prostate problems.
- Functional Incontinence means your bladder is functioning normally. Still, you may have a physical or mental limitation, such as arthritis or Alzheimer’s disease, that doesn’t permit you to react or move quickly enough to make it to the toilet. It also includes any urinary issues that impair your quality of life.
- Temporary Urinary Incontinence occurs when particular food, drinks, or medications are in your system and stimulate your bladder more frequently than usual. These include:
- Alcohol
- Caffeine
- Tea and coffee, whether regular or decaffeinated
- Soda and other carbonated beverages
- Artificial sweeteners
- Corn syrup
- Foods and beverages that are spicy, sugary, or acidic, particularly citric fruits
- Heart and blood pressure pills, muscle relaxants, and sedatives
- Large doses of vitamins B or C
- Urinary tract infection
- Constipation
With Testing Comes Diagnosis
Gynecologist performs a history and physical on you to rule out other diseases or ailments that might be causing your bladder problems. There’s also a basic physical test to see how well your bladder holds: close your mouth, pinch your nose and exhale as hard as you can. But many other tests can tell your doctor how your bladder is functioning.
Among things your doctor can do to rule more serious conditions out:
- Urinalysis
- Keeping a bladder diary, where you track your eating and drinking habits, as well as the frequency of your incontinence episodes
- Post-void residual measurement, a test where the gynecologist asks you to urinate into a cup to see how much your bladder is voiding on its own and then does a test to see if there is any urine left in your bladder
- Urodynamic testing involves a catheter that fills your bladder with water and measures the pressure of your bladder during filling and emptying the bladder.
- Cystoscopy, which uses a tiny tube with a lens that’s inserted into your urethra so the gynecologist can note or even remove any abnormalities occurring in your urinary tract
- Cystogram also uses a tiny tube inserted into your urethra; however, in this test, the doctor injects dye and traces it through X-ray imaging to see how your bladder expels liquid.
- Pelvic ultrasound, which checks for physical abnormalities of your organs and pelvis
Treatments: From Least to Most Invasive
- Bladder training, where you train your body to go longer and longer between bathroom breaks
- Double voiding — going to the bathroom, waiting a few moments to see how your body feels, then trying to go again to ensure an empty bladder.
- Scheduling your trips to the bathroom
- Managing your food and fluid intake
- Kegel exercises to strengthen your pelvic floor muscles
- Electrical stimulation
- Medications such as anticholinergics, mirabegron, alpha-blockers, or topical estrogen cream
- Urethral insert, a tampon-like device that you insert before physical activities that triggers your incontinence
- Pessary, a stiff ring inserted into your vagina to hold your bladder up and prevent leaks
- Bulking material injections, Botox® injections, or nerve stimulators
Surgery is a gynecologist’s last resort. At this point, your doctor may perform:
- A sling procedure
- A bladder neck suspension
- A prolapse surgery
- An artificial urinary sphincter insertion
If all else fails or you prefer not to try the medicines or surgeries, you can always choose between wearing pads and protective garments or wearing a catheter.
Your gynecologist should evaluate symptoms with a thorough consultation and examination for an accurate diagnosis and treatment plan to exclude any serious underlying condition.
Have questions about Urinary Incontinence? Schedule an appointment with the best OB Gynecologist, and top-rated urinary incontinence specialist, today.
Updated on Sep 23, 2023 by Manhattan Women’s Health and Wellness
Best-in-class
New York Gynecology Clinic
Manhattan Specialty Care in the Press

Call now to make an appointment with our highly rated Manhattan Gynecology doctors regarding your health. We look forward to seeing you!
book online now
(212) 378-9985
New York City Locations:
Manhattan Women's Health & Wellness (Upper East Side)
983 Park Ave, Ste 1D17
New York, NY 10028
(212) 389-1904
Manhattan Women's Health & Wellness (Midtown)
56 W 45th St, Ste 815
New York, NY 10010
(212) 677-7654
Manhattan Women's Health & Wellness (Union Square)
55 W 17th St, Ste 104
New York, NY 10011
(212) 378-9985