Loop Electrosurgical Excision Procedure (LEEP)
 While your annual pelvic exam isn’t the highlight of your year, it’s still something you have to do. Most often, you’ll get a clean bill of health and get on with your life. But if you ever do get an abnormal result, you want to know what’s going on — and fast.
While your annual pelvic exam isn’t the highlight of your year, it’s still something you have to do. Most often, you’ll get a clean bill of health and get on with your life. But if you ever do get an abnormal result, you want to know what’s going on — and fast.
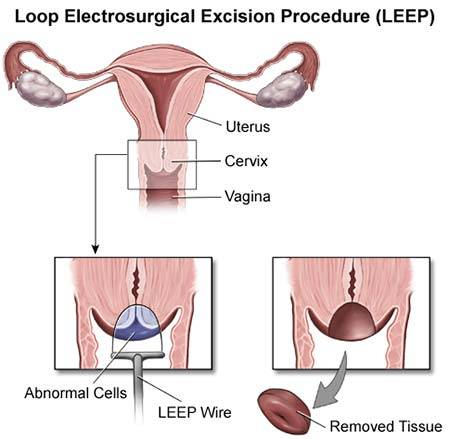
That’s when you might need to visit our center for gynecology in Manhattan for a loop electrosurgical excision procedure, otherwise known as a LEEP. When a cervical exam or Pap test reveals abnormal cells or growths, your gynecologist may order a cervical LEEP as a way to extract a biopsy, a thin amount of tissue, from the lower part of your genital tract, like from your cervix and/or vagina.
The LEEP tool is a thin wire loop through which an electric current passes. The device, heated by electricity, acts as a scalpel that can cut a thin layer of tissue off the surface of your cervix or vagina. Your doctor will send the tissue to a lab for analysis. After the LEEP has cut away abnormal tissue, the remaining healthy cells can continue to grow.
LEEP is an excellent procedure when encountering abnormal cells because it is not only diagnostic (identify) but can be therapeutic (treatment)
Why Is a LEEP Beneficial?
Our specialists use the LEEP because he wants to know if the abnormal cells discovered in your initial exam are cancerous, precancerous, or just a strange reading. A trained Manhattan gynecologist in Upper East Side and Midtown, New York can use the results to make an accurate diagnosis of your current condition. From the diagnosis, a treatment plan, if one is needed, can be put in place.
Other reasons doctors may want you to take a LEEP include testing for the following:
- Genital warts These are often benign but may point to a human papillomavirus infection. This test is called the HPV LEEP, and it’s essential because HPV is one of the early risk signs of cervical cancer. Just because you have genital warts doesn’t mean you have or are getting cancer, but your doctor wants to be sure.
- Endometrial polyps, which are always benign growths, can still interfere with your ability to get pregnant since they appear in your uterus and cervix. Your doctor can remove any large polyps with the LEEP.
- Diethylstilbestrol. It is the drug known as DES. According to the Centers for Disease Control and Prevention, 5 to 10 million pregnant women have taken DES in the mid-twentieth century. Still, it is now clear that DES raises the rate of reproductive system cancers.
How To Prepare for the LEEP?
You prepare for the LEEP as you would for a routine pelvic exam. It would be best if you didn’t undergo a LEEP during your period because your doctor needs a clear view of your cervix. Your doctor can perform the whole procedure in the office with it only taking a few minutes. A LEEP is often done on the cervix and sometimes performed on vagina walls or in the uterus. This procedure describes a cervical LEEP.
Your gynecologist places a speculum in your vagina to expose your cervix. A colposcope, positioned just outside your vagina, allows the doctor to get a clearer view. Then your cervix is cleaned and bathed in a vinegar solution, which turns any abnormal tissue white and may burn a little. Sometimes a Schiller test follows, in which your doctor dabs an additional iodine solution on your cervix.
Next, your doctor applies a local anesthetic to the area through a syringe. You may feel some discomfort, but you won’t feel any LEEP procedure pain. Once the drug is working, your doctor can begin the loop electrosurgical excision procedure.
How My LEEP Procedure has Carried Out?
Passing the LEEP wire loop through the speculum and into your vagina, your gynecologist may make several passes at your cervix to remove the abnormal tissue. During the LEEP, the electrical current cauterizes the blood vessels not to lose much blood. If you feel faint during this part of the procedure, tell your doctor because you must keep it as still possible while he works.
How much tissue doctors remove depends on the purpose of the LEEP. A biopsy requires very little tissue, but if the goal is to remove the abnormal tissue so healthy tissue can grow in its place, your doctor may have to remove more. When finished, a special paste can control any bleeding that the cauterization didn’t stop.
What To Expect After the Procedure?
While you rest, your gynecologist will send the tissue sample to a lab for analysis. If you bleed on the way home, your doctor will recommend that you wear a sanitary pad. You may need a mild pain reliever for the pain, but don’t take aspirin, which thins your blood and can encourage bleeding.
Other consequences of the LEEP include:
- Some cramping
- Red-pink spotting
- A blackish discharge, which comes from the paste used to stop the bleeding
All of these are normal and will stop in time. Follow your doctor’s instructions for your recovery. The guidelines you may receive include:
- Not douche or use tampons
- Abstain from sex after LEEP procedure for at least three or four days or as your doctor advises
- Avoid strenuous activities, such as jogging or heavy lifting
Your cervix may need two to four weeks to heal fully. Your OBGYN will let you know when to resume these activities and get back to your daily routine. You may need to get Pap tests more frequently in the future because an abnormal Pap after LEEP may mean you’ll have to undergo another loop electrosurgical excision procedure.
One of the options is performing the LEEP procedure while you comfortably sleep, so there is no discomfort felt during it.
Are There Any Side Effects?
The most common side effect from a LEEP during your recovery period is some heavier-than-normal bleeding. It’s usually not life-threatening. Your gynecologist can put more of the special paste on your cervix to stop it.
Contact your doctor right away if you notice any of the following symptoms:
- Fever with or without chills
- Bleeding that has clots
- Seepage from your vagina that smells bad
- Acute cramping or pain in your abdomen
Most women have no problem with pregnancy after LEEP, but there have been reports of a higher incidence of premature births or babies with lower-than-average weight. The LEEP rarely causes issues with your menstrual cycle, making it harder to get pregnant, but this is a rare occurrence.
Your gynecologist should evaluate symptoms with a thorough consultation and examination for an accurate diagnosis and treatment plan to exclude any serious underlying condition.
Important Reminder: The only intense of this information is to provide guidance, not definitive medical advice. Please consult the OB/GYN doctor about your specific condition. Only a trained, experienced gynecologist can determine an accurate diagnosis and proper treatment.
Do you have questions about Loop Electrosurgical Excision Procedure (LEEP)? Would you like to schedule an appointment with the best-rated New York City Gynecologist? Please contact our office.
Updated on Sep 23, 2023 by Manhattan Women’s Health and Wellness
Best-in-class
New York Gynecology Clinic
Manhattan Specialty Care in the Press

Call now to make an appointment with our highly rated Manhattan Gynecology doctors regarding your health. We look forward to seeing you!
book online now
(212) 378-9985
New York City Locations:
Manhattan Women's Health & Wellness (Upper East Side)
983 Park Ave, Ste 1D17
New York, NY 10028
(212) 389-1904
Manhattan Women's Health & Wellness (Midtown)
56 W 45th St, Ste 815
New York, NY 10010
(212) 677-7654
Manhattan Women's Health & Wellness (Union Square)
55 W 17th St, Ste 104
New York, NY 10011
(212) 378-9985