Manhattan Women’s Health and Wellness is a dynamic, modern obstetrics and gynecology practice delivering high-quality, individualized health care in multiple convenient locations in Manhattan. The OB-GYN center brings together a skilled medical team from the most prestigious medical schools in the country.
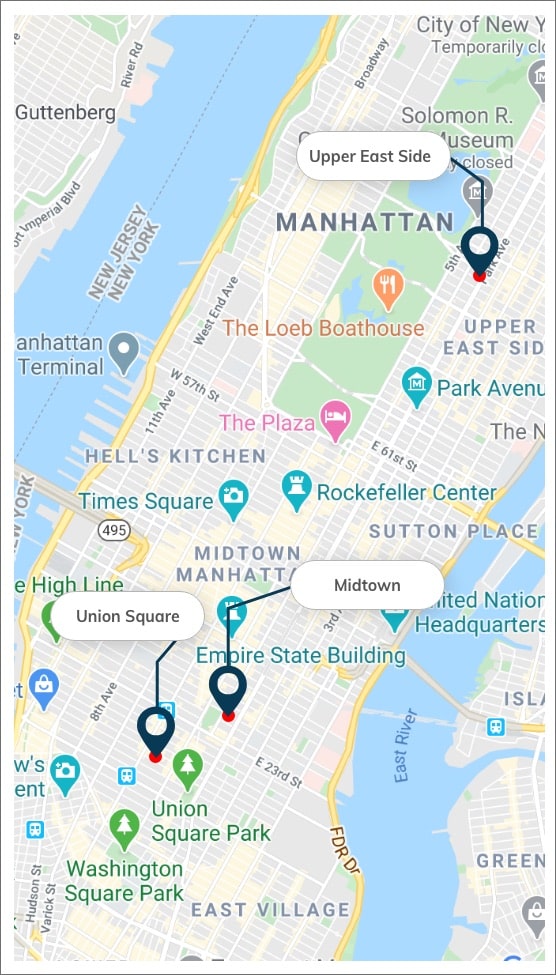
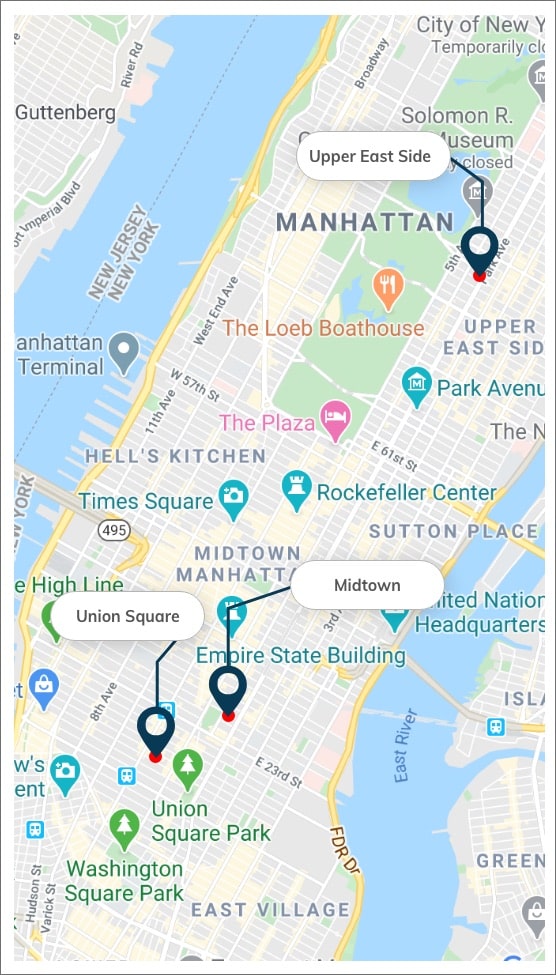
Our obstetricians-gynecologists serve women of all ages from all over New York, NY, and surrounding neighborhoods at their offices in Midtown, Manhattan, and Upper East Side, New York City. They are providing highly comprehensive gynaecology care in a safe, compassionate, and friendly environment. The physicians and exceptional health professionals deliver no less than a high-caliber quality of service. The experts working at our practice are among the best-known and most reputable obstetricians and gynecology specialists. The doctor-patient relationship philosophy is based on trust and has earned our healthcare providers one of the most respected reputations.
Our GYNs have the experience to diagnose your condition accurately using a time-tested, evidence-based approach. Our NYC gynecologist offers the least invasive FDA-approved treatments to women with urinary incontinence and prolapse of the pelvic organs, ensuring quick and painless recovery. Patients in Manhattan and the surrounding areas visit our neighborhood OB-GYN practice for a wide range of services, including medical advice/consultation, pelvic exam (bimanual examination), STDs, annual pap smear, and health issues related to female reproductive system health or infertility, such as uterine fibroids, endometriosis, PCOS, ovarian cysts, irregular menstruation, and vaginal infections.
The obstetrics and gynecology centers are certified and accredited by The Joint Commission. Our exceptional medical providers enhance the women's healthcare experience by utilizing the latest technologies, genetics, robotics, and molecular biology. Our OB/GYN doctors look forward to meeting you!